the ultimate guide to ROI in healthcare

When a single investment decision could save 100 lives, mastering healthcare ROI isn't just good business- it's an ethical imperative.
Healthcare ROI strategy has become a key skill for today's healthcare leaders. You know the tension if you've ever sat in a leadership meeting. On one side of the table, clinicians advocate for the latest diagnostic equipment that could catch diseases earlier. On the other hand, finance teams highlight shrinking margins and rising costs. In the middle? The fundamental question that keeps healthcare executives up at night: how do we prove that our investments in healthcare deliver measurable returns, both for our patients and our bottom line?
Understanding ROI in healthcare goes beyond traditional business metrics. Standard ROI formulas fall short when your ‘returns’ include saved lives, reduced pain, and healthier communities. You need a comprehensive healthcare ROI framework that captures both the financial realities of running a modern healthcare organization and the human impact of every decision you make.

what is ROI in healthcare?
Return on Investment (ROI) in healthcare represents the measurable benefits gained from investments in medical technology, processes, or programs relative to their costs. Unlike traditional business ROI calculations, healthcare ROI encompasses both financial returns and improved patient outcomes, making it a multifaceted metric that captures the true value of healthcare investments.
Also read: The ROI guide for healthcare marketers
why ROI in healthcare differs from other industries
The healthcare sector presents unique challenges when measuring ROI. While traditional industries focus primarily on financial returns, healthcare organizations must balance multiple objectives, including patient safety, clinical excellence, and community health improvement. This complexity requires sophisticated healthcare ROI metrics that capture both quantitative and qualitative value.
The key differentiators that set healthcare ROI apart from other industries are substantial and multifaceted. Healthcare investments must often meet specific regulatory requirements and compliance standards that directly affect ROI calculations, adding layers of complexity not found in other sectors.
the shift from volume-based to value-based care ROI
The healthcare industry is experiencing a fundamental transformation from volume-based reimbursement models to value-based care arrangements. This shift dramatically impacts how organizations calculate and optimize their healthcare ROI metrics, requiring a complete reimagining of traditional revenue models and success metrics.
In value-based care models, ROI calculations must account for quality metrics performance, where higher quality scores directly impact reimbursement rates and create financial incentives for excellence in patient care. Investments that lower the total cost of care generate positive ROI by reducing unnecessary utilization and improving care efficiency across the continuum.
Also read: a data-driven guide to enhancing ROI in healthcare access centers
why healthcare ROI metrics matter in modern healthcare
impact on strategic decision-making
Healthcare ROI metrics serve as the foundation for data-driven strategic planning. Organizations that effectively measure and analyze ROI can make informed decisions about resource allocation, service line development, and capital investments. These metrics enable leadership teams to prioritize initiatives that deliver the greatest value to both patients and the organization.
justifying technology and equipment investments
With healthcare technology costs rising, demonstrating clear ROI has become essential for securing approval for new investments. Whether implementing electronic health records (EHR) systems, purchasing advanced imaging equipment, or deploying telehealth platforms, healthcare leaders must present compelling ROI projections to justify expenditures.
demonstrating value to stakeholders
Healthcare organizations must satisfy diverse stakeholder groups, each with different perspectives on value. Comprehensive healthcare ROI metrics help communicate success across these varied audiences, ensuring that all constituents understand and support organizational initiatives. Board members typically focus on financial sustainability and strategic growth, requiring ROI metrics demonstrating long-term viability and competitive positioning.
healthcare ROI metrics for regulatory compliance
Regulatory requirements increasingly tie reimbursement to performance metrics, making ROI calculation essential for compliance and financial success. Organizations must track and optimize metrics across multiple programs and initiatives to maintain regulatory compliance while maximizing reimbursement opportunities.
Also read: Drive ROI and seamless consumer experiences with Contact Center
how to calculate ROI in healthcare
The fundamental healthcare ROI calculation follows the formula:
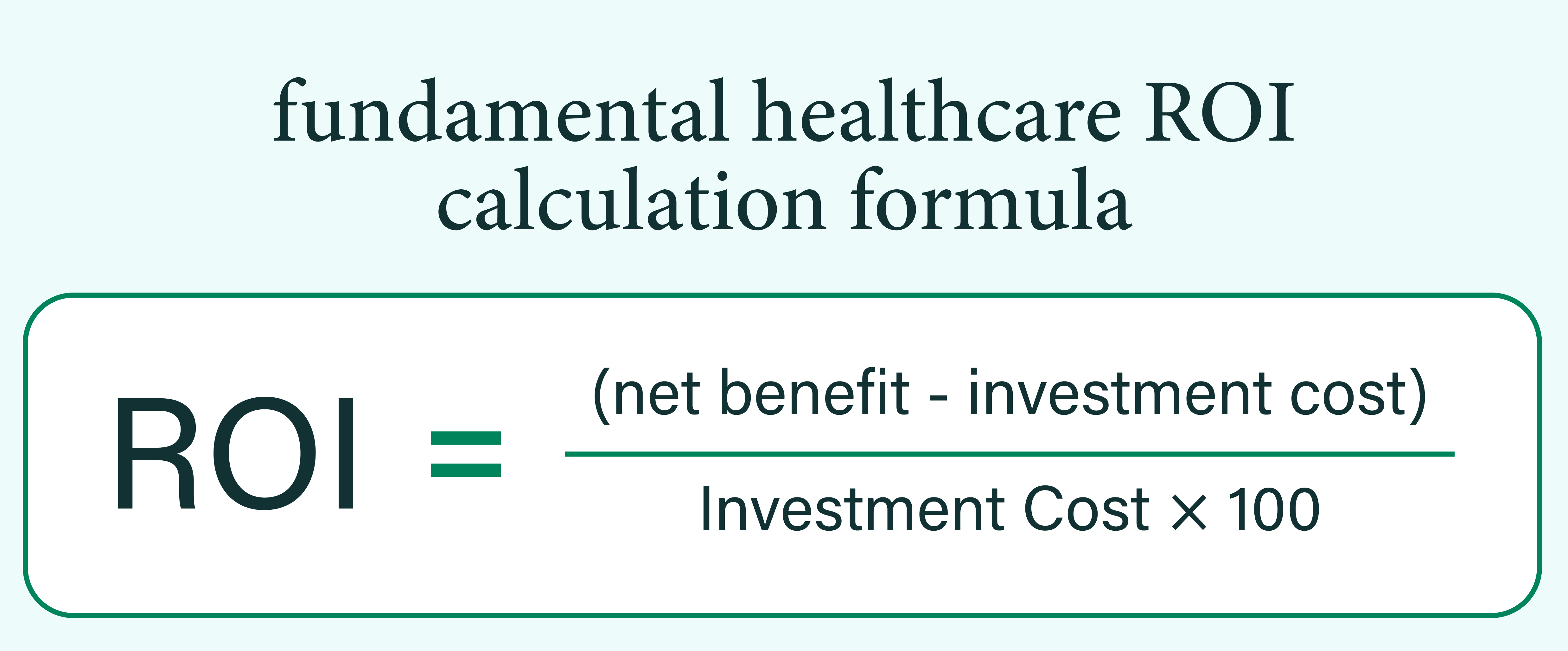
However, healthcare organizations often employ more sophisticated calculations that provide a more nuanced understanding of value creation in the complex healthcare environment.
Advanced ROI calculations in healthcare incorporate risk adjustment factors that account for patient population differences and case mix complexity. Time value of money considerations recognize that benefits realized in future years have different present values, requiring discounted cash flow analysis for long-term investments.
identifying costs (direct and indirect)
Accurate ROI calculation requires comprehensive cost identification that captures all resources consumed by an initiative or investment. Healthcare organizations must develop systematic approaches to cost accounting that ensure no significant expenses are overlooked in ROI calculations.
Direct costs are relatively straightforward to identify and include equipment purchase or lease expenses, software licensing and maintenance fees, staff salaries and benefits directly attributable to the initiative, training and implementation costs, and supplies and consumables required for ongoing operations. These tangible expenses form the foundation of ROI calculations but represent only part of the total investment picture.
Indirect costs often prove more challenging to quantify but can significantly impact true ROI. Opportunity costs of staff time diverted from other activities must be considered, as highly skilled clinical staff spending time on implementation reduces their availability for patient care. Workflow disruption during implementation can temporarily reduce productivity and efficiency, creating hidden costs that affect the entire organization.
measuring returns in healthcare settings
Healthcare returns manifest in various forms, requiring diverse measurement approaches that capture the full spectrum of value creation. Organizations must develop comprehensive measurement frameworks that track financial, clinical, and experiential returns to fully understand ROI.
Financial returns in healthcare include increased revenue from improved billing efficiency that reduces claim denials and accelerates payment cycles. Cost savings from reduced readmissions create immediate financial benefits while improving patient outcomes. Enhanced reimbursement from quality bonuses in value-based care programs provides additional revenue streams tied directly to performance improvement. Operational efficiency gains reduce per-unit costs of care delivery, improving margins while maintaining or enhancing quality.
Clinical returns represent the core mission of healthcare organizations and include improved patient outcomes and survival rates that demonstrate the effectiveness of clinical interventions. Reduced medical errors and adverse events not only improve patient safety but also reduce costs associated with extended stays and malpractice claims.
Experiential returns encompass the human elements of healthcare delivery, including higher patient satisfaction scores that drive patient loyalty and word-of-mouth referrals. Improved staff engagement and retention reduce recruitment and training costs while enhancing care quality through experienced teams. Enhanced organizational reputation attracts both patients and top talent, creating competitive advantages in the marketplace.
Also read: campaign planning 101: a healthcare marketers’ guide
common calculation mistakes to avoid
Healthcare organizations often encounter pitfalls when calculating ROI that can lead to poor decision-making and failed initiatives. Understanding and avoiding these common mistakes improve the accuracy and usefulness of ROI analyses.
Overlooking indirect costs represents one of the most frequent errors, as organizations fail to account for training time and workflow disruption that can substantially impact total investment requirements. Ignoring long-term maintenance needs leads to budget shortfalls when ongoing support and updates require resources not included in initial projections.
Overestimating adoption rates by assuming immediate full utilization of new technologies creates unrealistic ROI expectations that doom initiatives to perceived failure despite reasonable performance.
Neglecting risk factors by not accounting for implementation challenges or delays results in overly optimistic timelines and benefit projections. Focusing solely on financial metrics causes organizations to miss important quality and safety improvements that create substantial value even without immediate financial returns.
Don't let inadequate ROI measurement hold your organization back from achieving its full potential. Contact us today for a complimentary consultation and discover how optimized healthcare ROI metrics can drive transformational results for your patients, staff, and community.



